We don't often talk about our ovaries. But when you consider that 1 in 10 women are affected by polycystic ovary syndrome (PCOS), it's clear that we need to.
Just like 1 in 10 people are left-handed, or 1 in 12 have asthma — are we not talking about PCOS because we're not immediately affected by it? Maybe. But how do you know you're not?
Many women don’t find out that they have PCOS until they are actively trying to get pregnant, have trouble, and then look to get their fertility hormones tested. In fact, research estimates that about 70% of women with PCOS are either misdiagnosed or undiagnosed [1].
We deserve this information, and we deserve it much earlier in life — so, let's dive into it.
What is PCOS?
PCOS is a condition where your reproductive hormones, more specifically, androgens (male hormones, like testosterone and DHEA) are out of balance, encouraging your ovaries to produce way more androgens than they should [2].
What causes PCOS?
Studies have not been conclusive about how some women get PCOS and others don't, but researchers believe there are 2 things that can play a role:
- Genetics: Women who have relatives with PCOS are more likely to also have it [3].
- Insulin resistance: When insulin isn't working effectively, the body produces more of it. When there’s more insulin hanging out in the blood, this can increase the production of androgens, causing an imbalance of hormones.
How is PCOS diagnosed?
In Australia, the most widely accepted criteria for diagnosing PCOS is known as the Rotterdam Criteria 2003 [4][5].
According to this criteria, if you show 2 out of 3 of the following symptoms, it is grounds for a diagnosis:
- Irregular periods: Does your period sometimes come more than 35 days apart? Does it sometimes come less than 21 days apart?
- Increased androgens: Usually shown by excess hair growth (hirsutism), acne or raised testosterone levels in blood tests [6].
- Many immature follicles (known as cysts): These would be found on your ovaries via ultrasound and are known as polycystic ovaries.
What? Cysts on my ovaries?
For women who want to fall pregnant, getting told they have PCOS can feel like they've just been passed a fertility bomb.
Despite its damning name, you can still have PCOS and not have cysts on your ovaries. But if you do, this is what’s happening.
Your ovaries are filled with immature follicles. Each month, a small group of these follicles are told by your reproductive hormones that they need to start growing. If you ovulate, one of those follicles emerges as the dominant one — larger than the others — and basically tells the other follicles to take a hike.
However, if you don’t ovulate (which is sometimes what happens with PCOS), then you will not form a dominant follicle or suppress the other ones. Instead, the other follicles will keep on growing a little bit, and the problem with this is that you end up with many small, undeveloped follicles, which are called 'cysts.' This is what shows up in your ultrasound.
Normal ovaries

PCOS Ovaries

What are the symptoms of PCOS?
Symptoms can be different for every woman. You could experience one or a combination of the following:
Bear in mind, if you're currently using hormonal contraceptives, these symptoms can be masked. As soon as you come off the contraception, you might start noticing them again. Also, if you had any of these symptoms before you went on hormonal contraception, they may still persist once you come off it.
As we mentioned earlier, PCOS is a commonly misdiagnosed or undiagnosed condition. This becomes a bigger problem beyond your fertility if it's not managed properly. In fact, poorly managed PCOS can sometimes lead to lifelong increased health risks, such as type 2 diabetes, heart disease, endometrial cancer, and high blood pressure [7][8].
It's important that if you have PCOS, or suspect you may have it, you build relationships with doctors who are experienced and well-versed in the condition.
How does PCOS impact my fertility?
Women with PCOS have irregular ovulation. This makes it hard to predict the timing of ovulation, if it happens at all. Why does this matter? Well, in order to get pregnant you need 4 things:
- An egg to release (ovulate)
- At least one open, healthy fallopian tube
- Sperm to fertilise the egg
- A receptive uterus
Most women with PCOS will take longer to get pregnant because they might only release an egg every couple of months or perhaps not at all. But, there are options you can take to kickstart or regulate ovulation (more on this later!).
The most important thing to remember is, PCOS is not a life-long fertility sentence, and many women with it go on to have healthy pregnancies and deliver healthy babies.
How to manage PCOS symptoms
If you have PCOS and are struggling with any of the symptoms we mentioned earlier, the first thing you need to do is make some lifestyle changes [9][10].
Maintain a healthy weight
Studies have shown that weight loss of 5-10% can make a big difference in:
- Reducing insulin resistance
- Regulating your menstrual cycle
- Restoring ovulation [11]
- Reducing testosterone (and improving hair and acne)
- Improving your emotional and physical health
Even the most anti-gym goer can admit — that is a lot in return for a max of 40 minutes of moderate exercise every day [12].
Experts typically look at this based on your BMI, a number calculated by considering your weight-to-height ratio and that you can easily discover using an online BMI calculator, like Juniper's.
Generally speaking, the goal is to get your BMI to a healthy range, between 20-25 [13]. With this in mind, if you need to reduce your BMI, you should aim for around 40 minutes a day at moderate intensity. If you want to maintain it, around 20 minutes a day at moderate intensity should suffice.
And one extra tip: if you’re new to exercising, start small. Every bit of physical activity helps, even a brisk walk around the block. As you build your fitness up, you can try new and more challenging things: Pilates, boxing, weight training, barre — you name it.
There's no right or wrong way to approach an exercise regime for PCOS. It's simply about finding what you enjoy, so you actually stick to it.
Change to a PCOS-friendly diet
We don't like the word diet either, but research has found that what women eat can significantly help manage PCOS symptoms like acne, weight gain, and fertility [14].
Generally speaking, women with PCOS have elevated insulin levels or insulin resistance, so being able to adjust your diet to keep these levels stable is key to reducing the impact of PCOS symptoms.
Studies have actually shown that a low-GI diet can help your insulin levels behave [15].
GI (short for glycemic index) measures how quickly a particular food raises blood sugar levels.
A low-GI diet consists of eating foods that raise blood sugar levels slowly — like steel-cut oats — which help prevent insulin spikes and improve insulin resistance. You might want to introduce some anti-inflammatory foods too, as they can assist with fatigue.
To make your meal planning a bit easier, we've broken this down into your own cheat guide. It's pretty simple and there is nothing revolutionary — just a bunch of natural whole foods and not a huge deal of processed and packaged foods — but will make you feel a lot better.

Consider joining a weight loss program
If you’re struggling with these changes and need some help with early weight loss, joining a holistic weight loss program may just give you the push you need.
Juniper's Weight Reset Program combines prescription medication with unlimited follow-up consultations, health coaching, and 1:1 health tracking, so you can lose weight and actually keep it off.
Fertility treatment options
For those with PCOS who've been trying for a baby without success, there are 2 main fertility treatments to consider.
Ovulation induction
If you're not ovulating regularly and your BMI is below 35, there are safe medications that can be prescribed to help you release eggs more regularly.
Ovulation induction is a treatment that you can take orally or by injection at the beginning of your menstrual cycle and it works by stimulating the ovary to start or regulate your ovulation.
Your doctor will monitor this treatment carefully by ultrasound and blood tests so they can tell you when you are due to ovulate, and this will help you work out when it's the best time to schedule baby-making sex.
IVF
In Vitro Fertilisation (known as IVF) can be another option for some women. It's the most effective fertility treatment available, but it's still not guaranteed to work and can be expensive.
The process of IVF starts with injecting fertility drugs to help stimulate your ovaries to start maturing as many eggs as possible. As many eggs as possible are then retrieved from the ovaries with a simple procedure, and combined with sperm in the clinic to fertilise them — with the hope that some embryos will form. If successful, one of these embryos is then transferred and implanted into the uterus.
But before you go down the IVF path, there are a number of things you should consider to decide whether it is right for you.
Once pregnant, can PCOS complicate my pregnancy?
Unfortunately, it can.
PCOS increases your risk of some pregnancy complications such as gestational diabetes, high blood pressure, and miscarriage, which is why obstetricians will screen women with PCOS for diabetes when they become pregnant, and check in again later down the track (between 24 and 28 weeks).
What if I'm diagnosed with gestational diabetes?
Most pregnant women can maintain good blood sugar levels with diet and exercise. If you're diagnosed, have a chat with your GP or obstetrician so they can help you manage or reduce the risk of complications by monitoring your blood sugar levels and other tell-tale symptoms.
Now, let's talk weight for a second. A touchy subject, we know, but when you're pregnant with PCOS, you need to be strict about a weight gain goal.
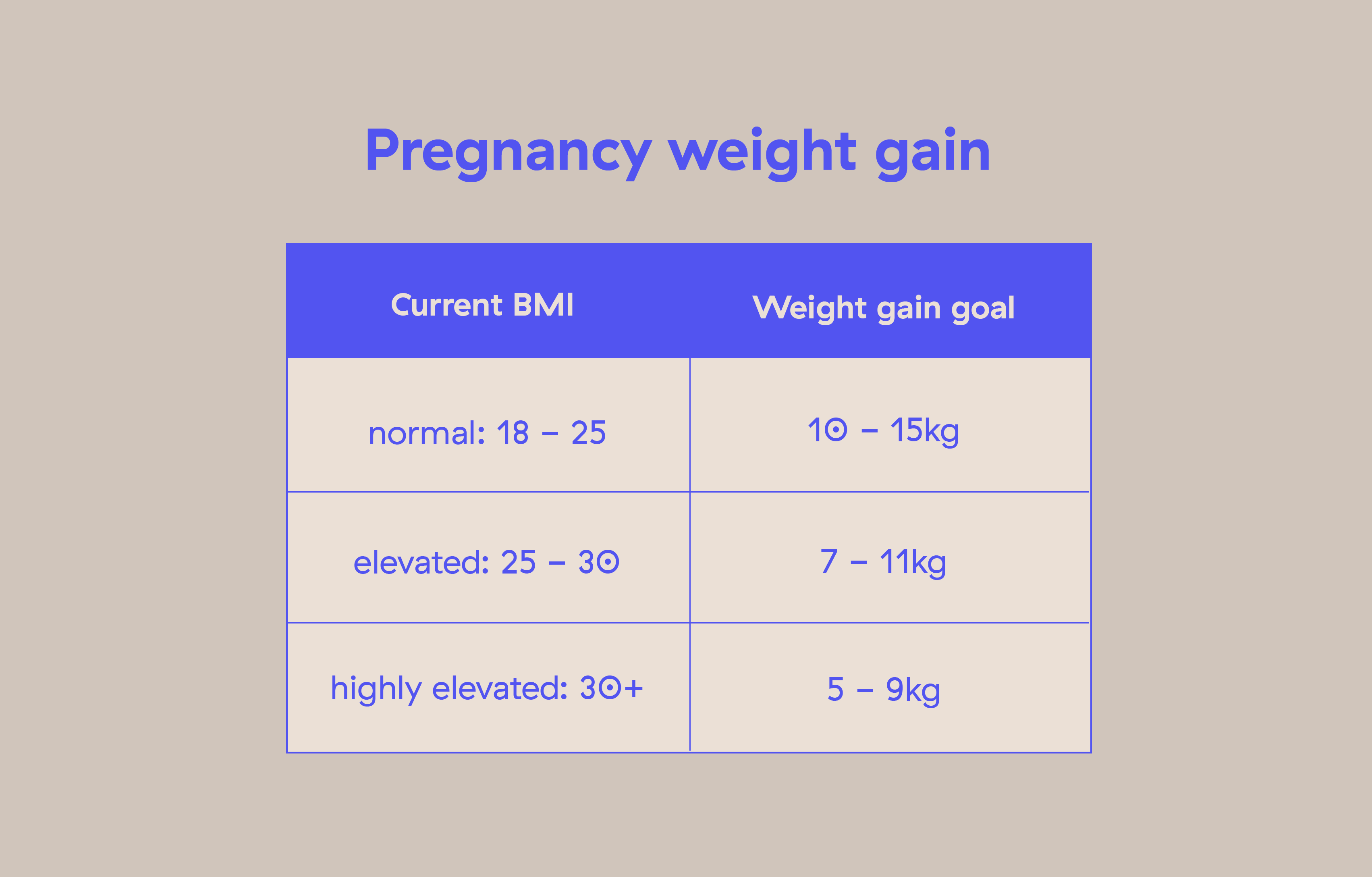
The best way to stay within your goal? Walking. Even if it's just a light 30-minute walk each day — it will make a bigger difference than you may realise.
Managing other PCOS symptoms
Depending on your symptoms, there are things you can do to improve your well-being while living with PCOS. These include:
Hormonal contraceptives for acne and hair growth
Hormonal contraceptives can help you balance out the reproductive hormones (in particular, reducing androgens) in your body. This helps manage PCOS symptoms like acne and excessive hair growth.
Hormonal contraceptives include the pill, patch, ring, the Depo Provera shot, implants (like Implanon), and hormonal IUD. Not all of them will be suitable for you, so it's a good idea to chat with your doctor before you make your choice.
If the pill is the right fit for you, Kin's birth control subscription is the easiest way for you to get it. It includes free and fast delivery of your contraception straight to your door, 2 weeks before you run out or even earlier if you prefer.
This also means no more trips to the doctors or chemist — simply complete a text-based consult with our Aussie practitioners and you'll have your pill in no time.
Mental health awareness and professional help
If you're getting into a tough headspace due to your PCOS symptoms, just know that you've got this. It's frustrating as hell, but it's also in your control [15].
We believe there is strength in knowledge and in understanding what's happening in your body and what you can do about it.
Additionally, keep reminding yourself that you’re not alone in this (remember, 1 in 10!). Getting support from your friends, family or health professionals early on can help ease the very real emotions you’re experiencing.
LYSN is a great online platform that puts you in touch with psychologists without having to leave the house, but if you want to see someone in person, there’s a Mental Health Care Plan that you may be able to access if you're in Australia and have Medicare.
We suggest you talk to your doctor about it so they can find out whether you're eligible. If you are, you’ll be entitled to access 6-10 sessions with a psychologist per year.
You're not alone
No doubt, PCOS can be a confusing and overwhelming diagnosis to receive. But as you can see, there's plenty you can do to take back control.
There's even a community that has been created by people with PCOS to share their experiences and support each other. They call themselves "cysters" (um, amazing) and often find each other online, through websites like Soul Cysters, Facebook groups and awareness-raising organisations. So, why not get amongst it?
At the very least, find a doctor, endocrinologist or fertility specialist who you trust to help you manage and understand PCOS. You've got this.
Image credit: Getty Images

















.svg)