In a nutshell
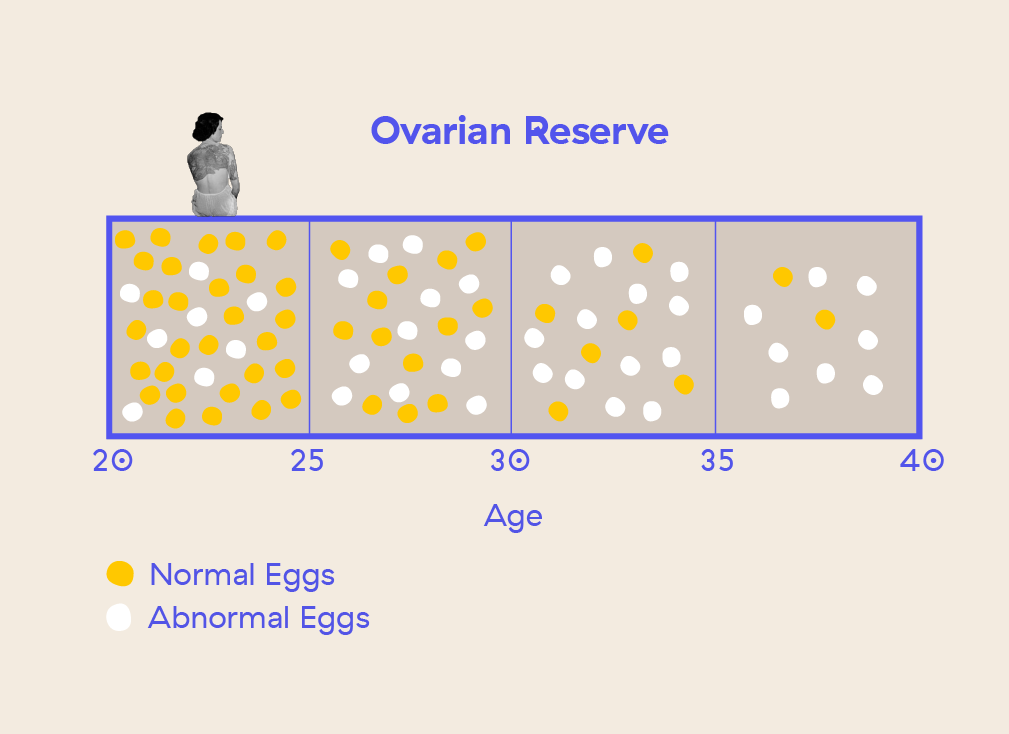
- Age is the most influential factor when it comes to your fertility health. Our most reproductive years are in our 20s. In our early 30s, our fertility starts to really decline. It starts to decline even more once we hit our mid-30s.
- During your late 30s or early 40s you are most likely to still have eggs, but the majority of them are likely to be abnormal. This increases your chances of miscarrying or having a baby with chromosomal abnormalities such as Down Syndrome.
- The more healthy eggs you have, the more likely that the egg that ovulates is a healthy one, and turns into a healthy pregnancy.
- The best hormone that can indicate your egg count is AMH (Anti-Mullerian Hormone).
Another year older
It’s one of the first questions that comes up about fertility: how old should you be when you have your first child? Well, there’s not really a magic number but there are statistics and hard truth facts you should be aware of.
What you might find interesting (or confronting) is that on average, Aussie women are having their first child at 31 years old.
Whether you’re single, in a stable relationship or maybe ending one, you might be looking at this number differently. Even if we were so sure we’d be having kids by a certain age, you’ll know by now that life plans can go to shit sometimes. And that’s okay.
We’re not going to sugarcoat this one, age is an incredibly important factor when it comes to your fertility journey.
But, what matters is that you take the time to get to know what your options are and understand the ins and outs of the biological clock chat.
Age matters for fertility
When it comes to your fertility, our most reproductive years are in our 20s. In our early 30s, our fertility starts to really decline. It starts to decline even more once we hit our mid-30s.
That’s right. As the number of candles on our birthday cake increases, our number of eggs decrease. Not the happiest of metaphors, but you can’t argue with science right?
Even if you look or feel great (which does impact your fertility in positive ways), your ovaries know exactly how old you are.
There’s no escaping it, age is the biggest influencing factor when it comes to your fertility. But how much exactly do our chances of pregnancy decline?
How age factors into your fertility
As you age, the quantity and the quality of your eggs decline. Both matter and neither can be reversed.
It’s harder to fall pregnant
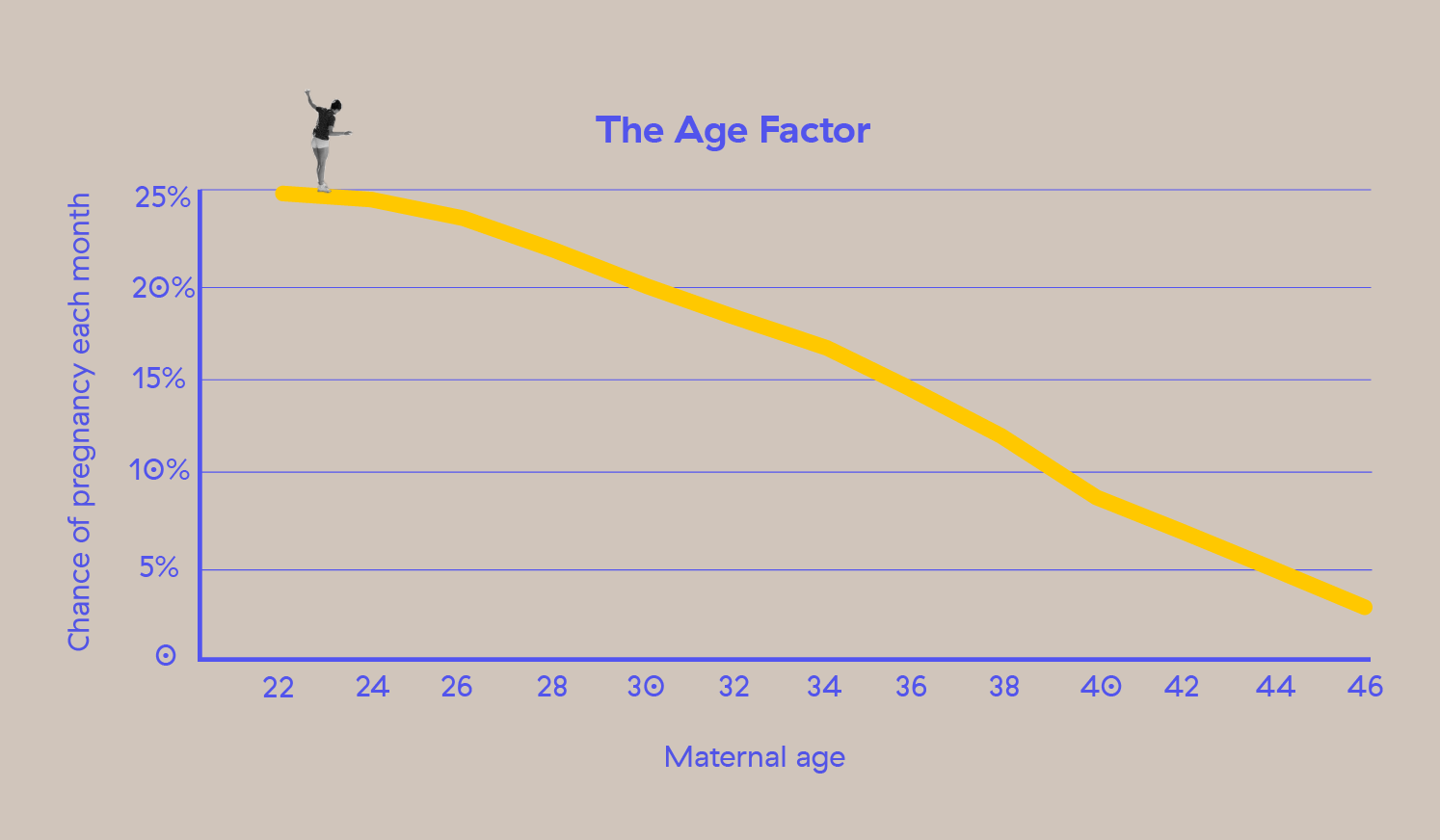
Our chances of conceiving every month is not 100%. For a healthy woman in her 20s, the chances of conceiving each month is 25%.
This declines to 20% by the time you’re 30. But, by 40 years old, our chances of getting pregnant every month are around 5% per cycle.
The risk of miscarriage rises
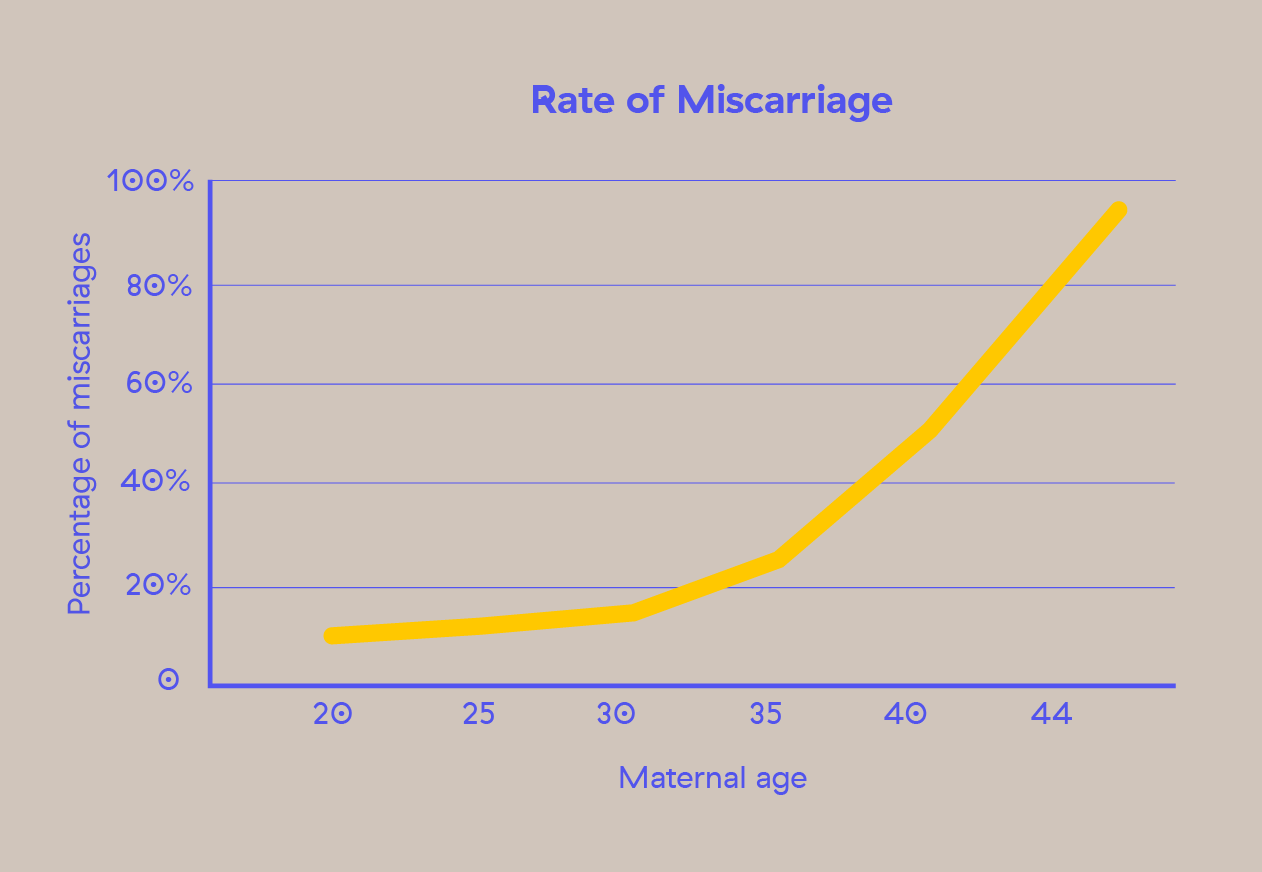
The risk of miscarriage rises as a woman ages, with a dramatic rise starting after age 35.
Chromosome abnormalities can happen
As we grow older, the chances that our eggs will be abnormal increase (more on that later).
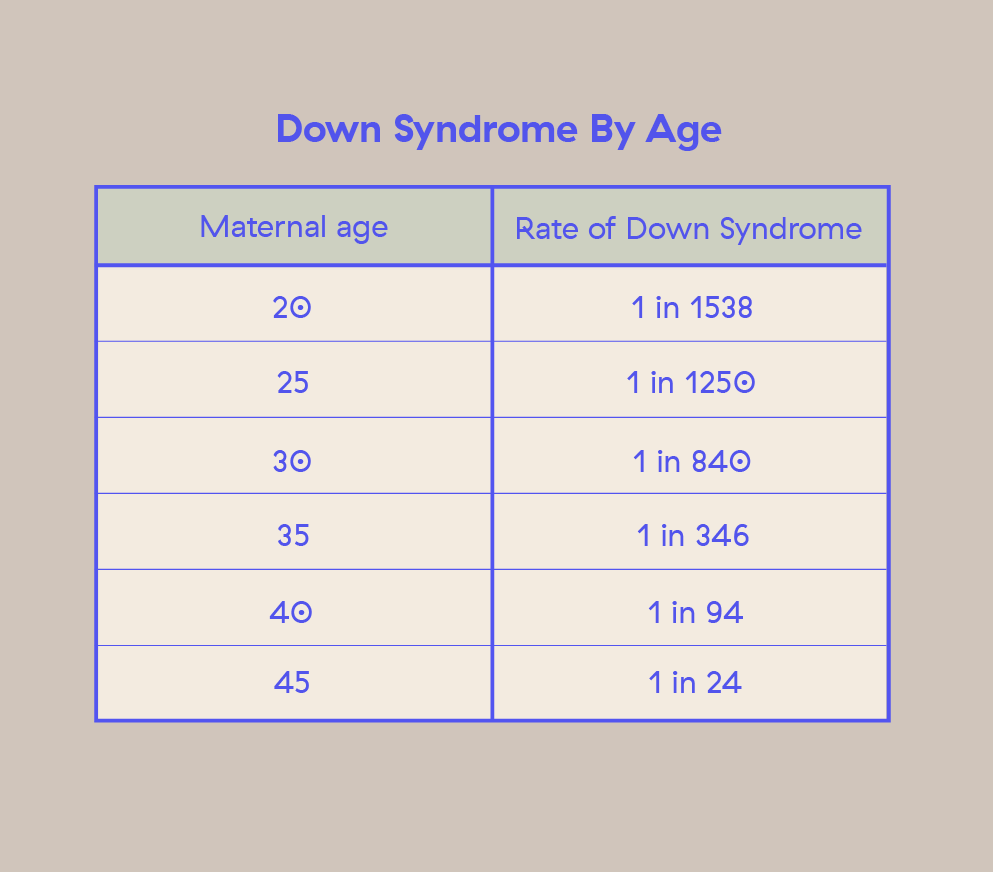
When an abnormal egg is fertilised, the embryo is more prone to chromosomal abnormalities, such as Down Syndrome.
IVF success rates decline
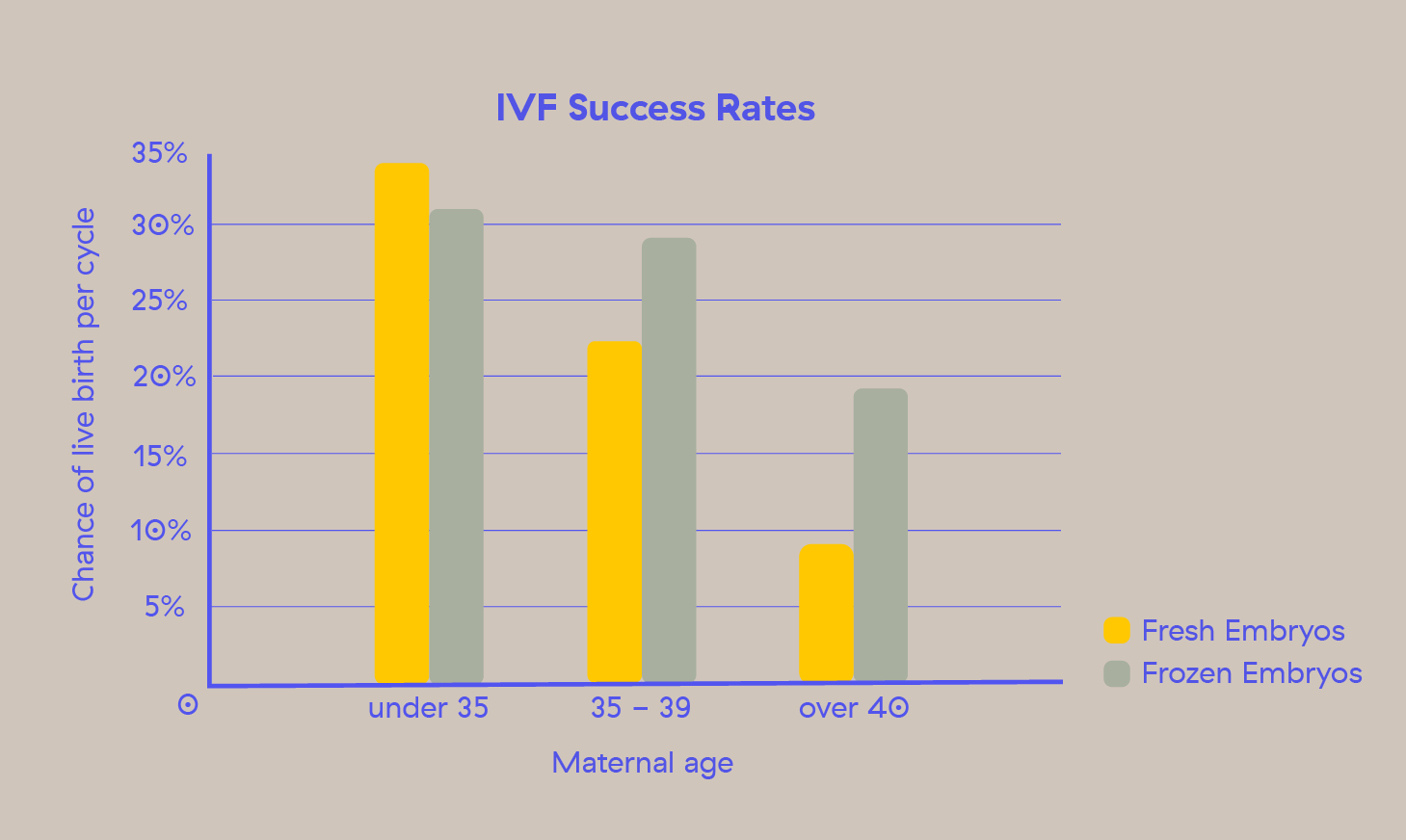
Surely we’re fine now that we have IVF as an option? We thought so too, but that’s not the case.
IVF success rates decline as you get older. This holds for whether you freeze your embryos or use them fresh.
Don’t compare yourself
Alright, let’s take a breather. We’ve put some pretty big discussion points on the table about fertility and ageing effects.
But like we said, your fertility doesn’t just fall off a cliff by the time you’re 35.
Every woman’s fertility curve is different, every woman’s body is different and so are her eggs.
The rate at which we lose our eggs also varies person to person. In rare cases, some women experience early menopause, where they have almost no eggs left around the age of 40 or earlier.
The rate at which the quality of our eggs depletes is also different. The more our eggs are exposed to smoking, for example, the greater the chances that our eggs will be abnormal.
Counting your eggs
We are born with 1-2 million eggs. That’s all the eggs we’ll ever have (this is called our ‘ovarian reserve’). Sure, that sounds like enough, but hitting puberty brings our egg count down to around 400,000.
So, where have all my eggs gone? Spoiler alert: It’s the whole age thing coming back to haunt you. That’s still 400,000 chances to get pregnant, right? Not quite.
Only about 300-500 of these eggs will mature enough to have the chance to roll down to funky town and get us pregnant. During each menstrual cycle, several follicles (fluid-sacs containing eggs) are recruited to prepare for ovulation. That’s right, multiple eggs.
But there is only one follicle that emerges as the ‘dominant’ one, containing the chosen egg.
Once that egg is released (the process we call ovulation), the rest of the eggs are sayonara too. No egg wants to be left behind so this number accelerates as we get older.
Your number of eggs continues to tick down until almost zero eggs are left. And you can’t ever get those eggs back.
That’s when we hit menopause. Menopause happens when your ovaries can no longer release an egg because we have almost none left.
At this point, you won’t be able to conceive naturally, because you'll no longer ovulate an egg.
What’s a healthy egg?
When it comes to your egg, quality is so key – it determines the likelihood of an egg being able to work with a sperm to produce an embryo.
As we age, so do our ovaries and every egg inside of them.
Let’s first talk about what we mean by ‘egg quality.’ Our eggs become more chromosomally abnormal as we age. As you ovulate, the egg cells go through a process of cell division.
This is known as meiosis, where the chromosomes split in half. Each parent gives an equal number of chromosomes to a pregnancy. But when the eggs are abnormal, the chromosome split is uneven.
This can lead to an embryo missing a chromosome or having an extra chromosome. Egg quality is fairly black and white too - either an egg is genetically normal (euploid) or it’s not (aneuploid).
Once an egg becomes abnormal, it can’t turn back time and become normal again.
So, as we age, a higher percentage of our eggs become abnormal.
Why does this matter?
Every month during our menstrual cycle, we ovulate one egg. This is our one chance to fall pregnant in that cycle. That same egg may be normal or abnormal.
If it’s a normal egg: Sweet. You’re off to a great start for a healthy pregnancy.
If it’s an abnormal egg: Things get tricky. They are typically less likely to become fertilised with sperm or implant on your uterus - both of which you need to achieve a natural pregnancy.
In the rare case that a pregnancy is achieved (based on the age stats), you have a higher risk of miscarriage. If the egg leads to a live birth, it may result in genetic disorders in the child, like Down Syndrome.
Investigate your eggs
You can’t test for the quality of your eggs, but you can do a test to understand more about the quantity of your eggs.
The best indicator for the quality of your eggs is your age.
On average, women in their early 20s have approximately 20% abnormal eggs, while women in their 40s have upwards of 60% abnormal eggs.
What’s my egg count?
There are hormone tests you can take to check out how many eggs you’ve got chilling in your ovaries.
Three main hormones can indicate your egg count (or ovarian reserve):
- AMH (Anti-Mullerian Hormone)
- FSH (Follicle Stimulating Hormone)
- E2 (Estradiol)
To check the levels of these hormones in your blood, you will need to take a fertility test.
To learn more about these fertility tests, check out our Fertility Testing Guide.
Taking an AMH test
If you want to know your egg count, recent studies have shown AMH is the best indicator for your ovarian reserve.
AMH is the hormone that is produced by the cells inside your follicles (the sacs that carry your eggs).
The level of AMH in your blood strongly correlates with the total number of follicles inside your ovaries, and therefore, your total egg count.
As a bonus, your AMH can also give you a clue as to when you’re likely to experience menopause and how your body will respond to procedures like IVF and egg freezing.
FSH can also give us an indication of our ovarian reserve, but it’s important to check E2 along with it, because high E2 levels can suppress FSH. Meaning, if your FSH levels are suppressed by E2, the FSH measurement may not accurately represent your ovarian reserve.
While AMH is the best test for egg count, to get the most holistic and complete picture of ovarian reserve and fertility in general, it’s great to test for AMH and FSH and E2. The more data, the better.
Menopause isn’t the expiry date
We’re familiar with the term menopause. It’s technically the final age where your fertile clock stops ticking. You have almost no chance of conceiving naturally, because you have no eggs left to fertilise.
In Australia and New Zealand, the average age for menopause is around 51 years old. Take this with a grain of salt - as the average will vary based on multiple factors, including ethnicity and family history.
While you still have chances of getting pregnant until you reach menopause, it’s important to know that women actually start to lose their fertility 4 to 8 years before menopause.
It’s time to get familiar with the term perimenopause. This is when your body goes through a 4 to 8 year transition process into menopause.
During this period you could still have eggs, but the majority of them are likely to be abnormal. Plus, you're more likely to be ovulating irregularly. Both of which, significantly reduces your chances of conceiving a healthy baby.
What about men?
Yep, ageing affects male fertility as well, but not to the same extent that it does female fertility. Why is this?
It’s partly due to the fact that unlike women and their eggs, men’s bodies develop sperm constantly - sometimes more than 100-200 million fresh new swimmers each day!
But, conception is 30% less likely for men over the age of 40 years as compared with men younger than age 30 years. As men age, semen motility (their ability to swim) and the actual volume of semen a man produces decreases.
On top of this, sperm becomes more and more abnormal as men age. This increases the chances of miscarriage, stillbirth and birth defects. So it really does take two to tango.
Freezing your eggs
Unfortunately no one is able to stop time, so you might consider freezing your eggs as a way to slow down your fertility clock. Or at least, stop your eggs from ageing.
Freezing your eggs is exactly what it sounds like. Your gynaecologist will collect a few of your eggs while you’re young(er) and freeze them in a lab until you’re ready to use them, effectively preserving egg quality.
It gives you the option to use it later down the track when you’re ready. When that time comes, your gynaecologist will combine it in a lab with sperm and place it back into your uterus. A process called IVF (in vitro fertilisation).
Freezing your eggs is a great option to give you options down the track.
But, it's equally important to know that it's not guaranteed to work, so it's not always the right decision for everyone. It can be expensive, physically invasive and emotionally and hormonally challenging.
There are questions you need to ask yourself before you decide to freeze your eggs.
So, what’s next?
We’re not getting any younger, but that doesn’t mean we are running out of options and can never get pregnant.
Sure, we can’t argue with science and turn back time on our fertility health. But what we can do is learn about our fertility health earlier in life. It’s the most powerful first step you can take to start taking control of your fertility.
Developed by fertility specialists, our Conception Checklist is tailored to your stage and lifestyle, and is designed to take the stress out of planning for a family, so that you can enjoy the journey rather than get lost in it.
















.svg)